Leobit Wins 2025 Cloud Computing Awards in Business Cloud Transformation Category
February 10, 2026How Legal Guidance Helps People Make Sense of Chaos after an Injury
February 10, 2026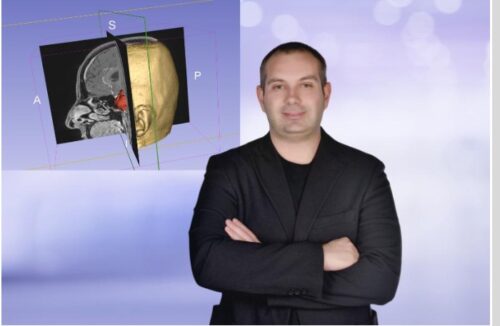
In modern neurosurgery, technology is not about sharpening the scalpel in the surgeon’s hand—it is about determining precisely where that scalpel must not touch. Segmentation (digital tissue differentiation) methods used in brain tumor surgery are not merely imaging techniques; they represent an efficiency model that directly impacts both patient quality of life and national healthcare economics.
The three-dimensional roadmap obtained through digital segmentation transforms surgery from a “surprise” into a predictable process. By minimizing the risk of unforeseen events—even in the most complex anatomical regions—it elevates patient safety to its highest level.
Brain tumor segmentation is a cornerstone of surgical planning and begins long before the operation itself. The process involves analyzing high-resolution magnetic resonance imaging (MRI) or computed tomography (CT) scans using specialized software. Radiologists and neurosurgeons meticulously delineate the tumor’s volume, shape, relationship to normal brain tissue, and proximity to critical anatomical structures such as major vessels and neural tracts.
This digital marking process separates the tumor from surrounding healthy tissue. Advanced computer algorithms then reconstruct two-dimensional slices into a comprehensive three-dimensional model of the tumor and its environment.
This 3D model provides the surgeon with a precise “roadmap” during surgery, clearly displaying the tumor’s location, depth, and adjacent sensitive structures. Integrated into neuronavigation systems in the operating room, this digital map allows the surgeon to work in real time with a virtual guide, enabling safer and more precise intervention.
Ultimately, segmentation is a critical step that enhances the surgical team’s understanding of the brain’s complex architecture, facilitates minimally invasive tumor removal, and maximizes preservation of healthy tissue.
Minimal Damage, Maximum Functional Preservation
In brain surgery, success is measured not only by tumor removal but by the functional integrity of the tissue left behind. Segmentation technology offers the surgeon a digital protective shield by differentiating tumor borders from normal brain parenchyma and vital vascular structures with millimetric precision.
When integrated into intraoperative neuronavigation systems, these high-resolution datasets help surgeons remain within “safe surgical margins,” minimizing error.
The most tangible economic reflection of this precision is the prevention of severe postoperative complications such as paralysis, speech disorders, or cognitive impairment—conditions that carry substantial treatment costs.
From a health economics perspective, every complication-free case represents avoided expenses: long-term rehabilitation, additional medications, prolonged care services, and repeated hospitalizations. By preserving healthy tissue, segmentation prevents enormous downstream costs before they even arise.
Efficient Use of Hospital Resources and Cost Savings
Precision segmentation fundamentally reshapes the postoperative recovery curve. When healthy brain tissue is carefully preserved, the brain recovers more rapidly from surgical trauma. This accelerates edema control and significantly reduces the need for intensive care.
Considering that surgical wards are among the highest-cost hospital units globally, shortened recovery times translate directly into major financial savings. For example, reducing hospitalization from seven days to three does not merely lower individual treatment costs—it increases hospital resource efficiency by over 50%, allowing more patients to receive care.
Shorter occupancy of high-cost surgical beds alleviates systemic bottlenecks. When complications are minimized, secondary costs such as rehabilitation are also effectively eliminated, resulting in comprehensive economic optimization.
Preventing Loss of Human Capital and Productivity
One of the most critical yet often overlooked parameters in health economics is productivity loss following surgery. For working-age individuals, brain surgery can be perceived as a potential end to an active professional life.
Segmentation’s millimetric precision protects motor and cognitive functions to the highest possible degree, enabling patients to return to their professional lives sooner and at full capacity. Accelerated return-to-work benefits not only individual income continuity and economic independence but also reduces the burden of disability payments on social security systems.
By preserving functional tissue, this technological approach acts as a strategic economic shield—protecting family finances at the micro level and safeguarding workforce productivity at the macro level.
Eliminating Invisible Costs: Technological Efficiency in Neurosurgery
Permanent deficits following brain surgery are not only medical complications; they may require a family member to leave work to become a caregiver, creating lifelong financial strain. This “hidden cost,” defined in health economics as workforce loss, can mean the end of a career for working-age patients.
Each neuron preserved through segmentation technology disrupts this negative cost chain. Functional preservation enables patients to return to professional life rapidly, protects family income, and reduces social welfare expenditures, thereby preventing national income loss at a macroeconomic scale.
In Turkey and worldwide, surgical services represent the highest-cost hospital units. A brain tumor surgery performed with millimetric preservation of healthy tissue not only enhances surgical success but also shortens hospital stay, producing significant savings in healthcare expenditures.
This technological approach eliminates secondary costs—home care services, lifelong medications, assistive medical devices—before they arise. Reducing hospitalization from seven days to three generates more than 50% resource efficiency in high-cost surgical units.
Digital precision in surgical artistry thus serves as a strategic economic safeguard: maximizing quality of life while minimizing additional rehabilitation costs imposed on the healthcare system.
Investment or Savings?
Access to segmentation technology may initially appear as an added expense for hospitals or patients. However, the “functional success” achieved through this investment returns its cost many times over.
The greatest savings in healthcare come from restoring patients to normal life as quickly as possible, with the least possible harm.
Caner Sarıkaya, MD
Department of Neurosurgery
Maltepe University Hospital
Istanbul, Turkey
E-mail: drcanersk@gmail.com
For further clinical insights and academic perspectives on modern brain and spine surgery, visit:
https://www.drcanersarikaya.com/
